Name Used to Describe Participating Providers in Bcbs Plans
Identify a method that BCBS uses to improve healthcare. Participating Provider Versus Non-Participating Out-of-Network Provider.
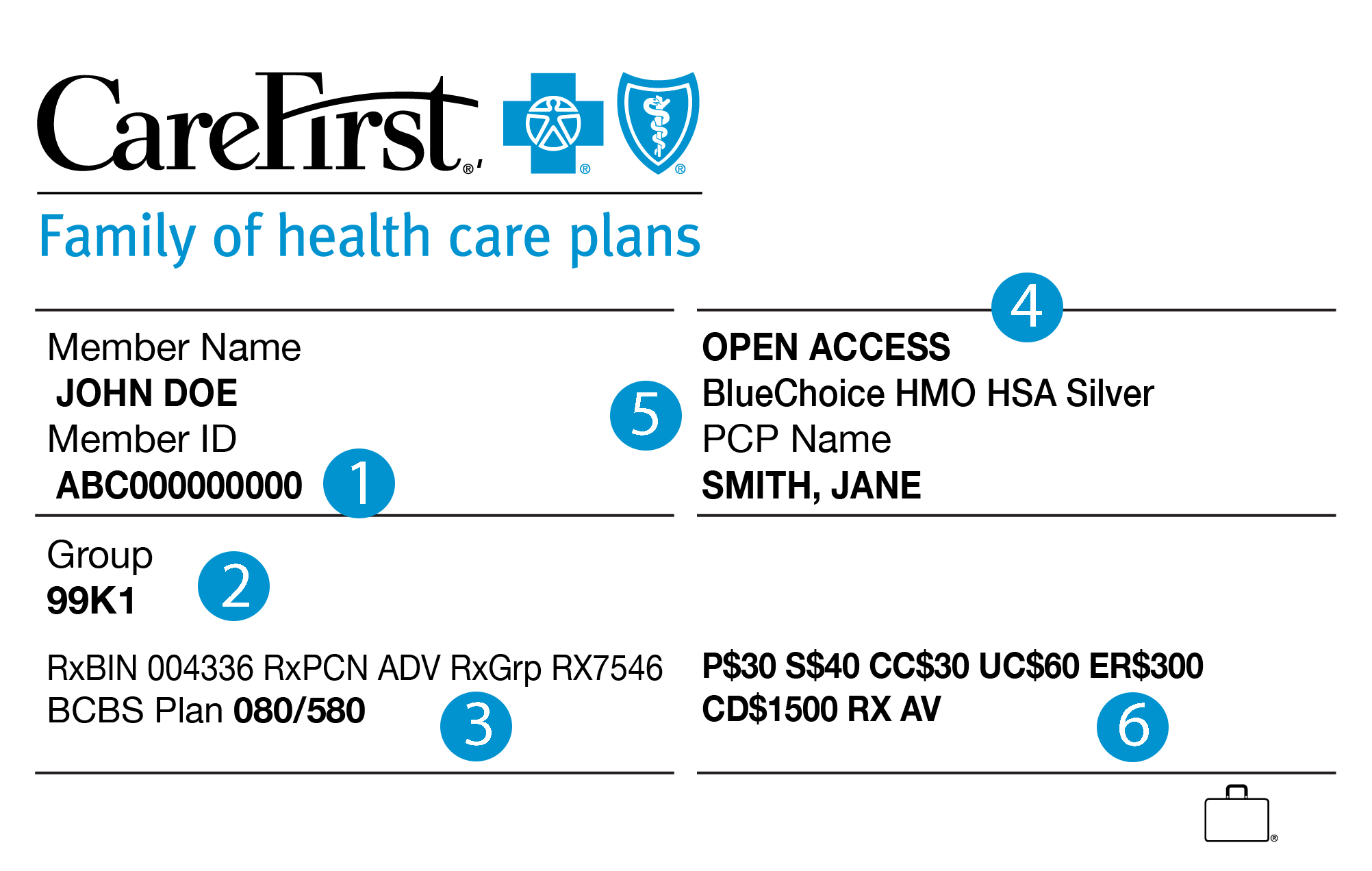
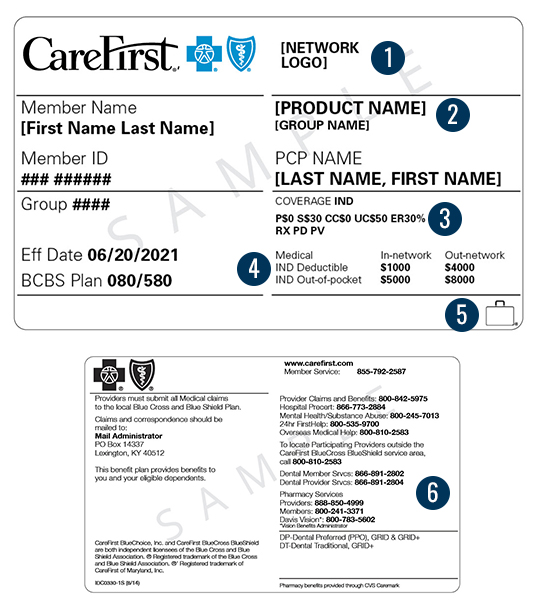
Your Member Id Card Carefirst Bluecross Blueshield
A member in an indemnity BCBS plan has an individual deductible of 500 and a family deductible of 1000 with a coinsurance rate of 90 percent after the deductible has been met up to an annual maximum out-of-pocket amount of 2000.
. Participating providers contract to participate in a BCBS plans preferred provider network PPN which is a program that requires providers to adhere to _____ care provisions. Identify the local BCBS plan in the providers service area where a claim is submitted after providing treatment. Name the term used to describe participating providers in BCBS plans.
Host Plan A Plan participating in the BlueCard Program that extends hospital andor medical care to a Blue Cross Blue Shield member. And CareFirst Advantage DSNP Inc. Refers to the use of providers who participate in the health plans provider network.
Serving Maryland the District of Columbia and portions of Virginia CareFirst BlueCross BlueShield is the shared business name of CareFirst of Maryland Inc. Identify the local BCBS plan in the providers service area where a claim is submitted after providing treatment. CareFirst BlueCross BlueShield Community Health Plan.
Many benefit plans encourage members to use participating in-network providers to reduce out-of-pocket expenses. CareFirst BlueCross BlueShield Medicare Advantage is the shared business name of CareFirst Advantage Inc. Your insurance carrier agrees to direct clients to the provider and in exchange the provider accepts a lower fee for their services.
Identify the local Blue Cross Blue Shield plan in the provider service area where a claim is submitted after providing treatment. Serving Maryland the District of Columbia and portions of Virginia CareFirst BlueCross BlueShield is the shared business name of CareFirst of Maryland Inc. Incidental Procedures Procedures carried out at the same time as a primary procedure that are clinically integral to the performance of the primary procedure.
Name the term used to describe participating providers in BCBS plans. And The Dental Network are independent licensees of the Blue Cross and Blue Shield Association. You pay less if you use providers that belong to the plans network.
Group Hospitalization and Medical Services Inc and First Care Inc. Identify the local BCBS plan in the providers service area where a claim is submitted after providing treatment. CareFirst BlueCross BlueShield Medicare Advantage is the shared business name of CareFirst Advantage Inc CareFirst Advantage PPO Inc.
Asked Aug 19. Serving Maryland the District of Columbia and portions of Virginia CareFirst BlueCross BlueShield is the shared business name of CareFirst of Maryland Inc. Identify an insurance service that private payers supply.
Host plan a patients _____ process the Blue Cross Blue Shield claim and sends it back to the host plan. Vaccines against certain diseases which can be administered either orally or by injection. Calculate the total amount the patient owes if.
24-hour coverage A plan under which an employers group health plan disability plan and workers compensation program are merged integrated or coordinated depending on state regulations into a single health. Asked Aug 19 2019 in Health Professions by Dragonella. A participating provider has contractually agreed to.
Network providers and preferred providers are both contracted in-network providers available to the members of the health plan. Many benefit plans encourage members to use. CareFirst BlueCross BlueShield Medicare Advantage is the business name of CareFirst Advantage Inc.
Name the term used to describe participating providers in. Identify the local BCBS plan in the service providers area where a claim is submitted after approving treatment. Many benefit plans encourage members to use participating in-network providers to reduce out-of-pocket expenses.
A member in an indemnity BCBS plan has a family deductible of 500 with a coinsurance rate of 70-30 after the deductible has been met up to an annual maximum out-of-pocket amount of 2000. A member in an indemnity BCBS plan has a deductible of 700 with a coinsurance rate of 90-10 after the deductible has been met up to an annual maximum out-of-pocket amount of 2000. First Care Inc CareFirst of Maryland Inc Group Hospitalization and Medical Services Inc CareFirst BlueChoice Inc.
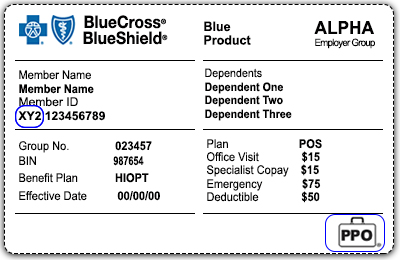
Claims for members of other Blue Cross andor Blue Shield Plans who receive hospital or medical care from a participating provider of Highmark Blue Cross Blue Shield of Western New York. A participating provider has contractually agreed to. Document issued to a covered member confirming his or her eligibility to claim benefits.
Blue Cross and Blue Shield companies also offer a consumer driven health plan called _____ Host plan. A member in an indemnity BCBS plan has a deductible of 700 with a coinsurance rate of 90-10 after the deductible has been met up to an annual maximum out-of-pocket amount of 2000. Participating Provider There are some similarities between preferred providers and what are known as participating providers but participating providers fall into a specific subset of.
Incidental Procedures Procedures carried out at the same time as a primary procedure that are clinically integral to the performance of the primary procedure. You can use doctors hospitals and providers outside of the network for an additional cost. And Group Hospitalization and Medical Services Inc.
The Blue Cross Blue Shield Association is an association of 35 independent locally operated Blue Cross andor Blue Shield companies. The Blue Cross and Blue Shield Names and Symbols are registered trademarks of the Blue Cross and Blue Shield Association. Name the term used to describe participating providers in BCBS plans.
Participating par providers are healthcare providers who have entered into an agreement with your insurance carrier. Preferred Provider Organization PPO A type of health plan that contracts with medical providers such as hospitals and doctors to create a network of participating providers. And Group Hospitalization and Medical Services Inc.
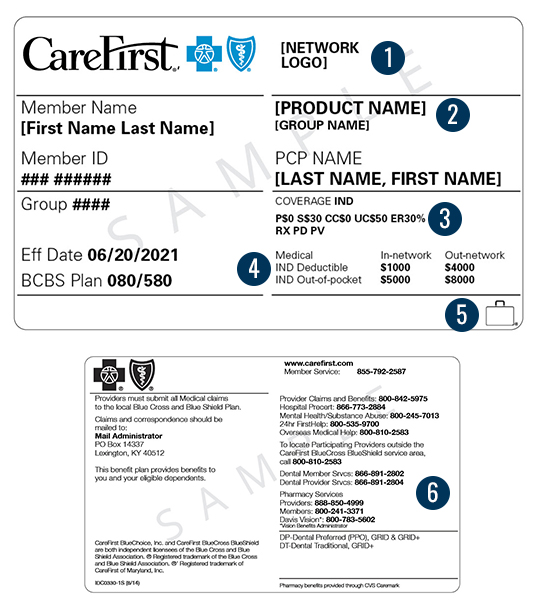
Member Id Card Carefirst Bluecross Blueshield

Comments
Post a Comment